Journal of Entrepreneurial Health Sciences and Innovation (JEHSI)™
COVID-19: Effectively Preventing Exercise Deficit
Disorder and Improving Mental Health
Dr Gabriel Pulido-Cejudo1,2*, Peter Humphries2 and Dr Khadija El Abdaimi1,2
1International Centre for Advancement of Health Regional Innovation and Science, ICAHRIS Research
*corresponding author, gabriel.pulido-cejudo@icahris.org
2Canadian Federation of Breast Diseases, CFBD
Abstract
The steady decline in physical activity in children and adult populations has led to the definition and characterization of the medical concept of exercise deficit disorder (EDD), a low level of physical activity that does not attain the minimal recommendations of daily exercise routines as prescribed by public health initiatives. This article provides a quantifiable framework for the early identification, prevention, and treatment of Exercise Deficit Disorder (EDD) aiming at reducing its impact on the onset of mental, cardiovascular, metabolic syndrome, obesity and chronic diseases such as Type 2 diabetes and cancer.
Keywords: COVID-19, Exercise Deficit Disorder, EDD, physical activity, public health, pandemic, identification, prevention, treatment
Article
Introduction
Nearly a decade ago and one year after our publication describing the epidemic onset of obesity and hyperobesity in north American children[1], the steady decline in physical activity in children and adult populations has led to the definition and characterization of the medical concept of exercise deficit disorder (EDD)[2,3]. Initially described as a low level of physical activity that does not attain the minimal recommendations of daily exercise routines as prescribed by public health initiatives[2,3], the recognition of EDD as a medical condition has proven to be an important tool to establish an effective clinical road map for its prevention and treatment. This article provides a quantifiable framework for the early identification, prevention, and treatment of Exercise Deficit Disorder (EDD) aiming at reducing its impact on the onset of mental, cardiovascular, metabolic syndrome, obesity, and chronic diseases such as Type 2 diabetes and cancer.
Early Detection of Exercise Deficit Disorder EDD
With few exceptions, lack of physical activity and daily exercise translates into reduced musculoskeletal function, inflammation, cardiovascular disorders, overweightness and obesity, being equally an underlining triggering factor of type 2 diabetes and cancer[1,4-6]. Less known is the direct impact of exercise deficit disorder in reduced gastrointestinal and sperm motility leading to, among other, constipation and infertility respectively[7-10]. Physical inactivity and the onset of Exercise Deficit Disorder (EDD) is also accompanied by various behavioural and mental health disorders including difficulties in socializing, anxiety, and depression[1-4,11].
Globally, during the last decade, a steady decrease in physical activity during the transition from adolescence into adulthood has proven to be an important triggering factor in decreased social development, mental health issues and the gradual onset of obesity in younger adults[1-4,11].
Physical inactivity and obesity have been considered to be the main causes of death in 10% to 13% of affected individuals in Europe, equally encompassing a global annual death toll of 2.8 million people within low to high income countries[12,13].
Although the concept of EDD as a medical condition was first proposed a decade ago[2-4], to date, no quantifiable set of parameters has been put together to clearly identify the early onset of this disorder.
After having created a comprehensive Global Preventive Health Platform in 2015, and apart from performing personalised blood tests and clinical profiles for individuals interested in addressing or improving their current health status, we have identified quantitative parameters for the identification of EDD. These are summarised in Table 1.
| Key Quantitative Parameters | ||
| Parameter | Average Normal | Average EDD |
| Weekly Minutes Combined Physical Activity (WMCPA) | ≥ 180 minutes | ≤ 90 minutes |
| Body Mass Index (BMI) | 22 | 27 |
| Waste-to-Hip Ratio (WHR) | ≤ 0.85 Women | ≤ 0.90 Men | ≥ 0.90 Women | ≥ 0.95 Men |
| Constipation | Rare (1-2 episodes a year) | Frequent (1-2 episodes a month) |
| Percentage of Maximum Heart Rate Reserve (HRR) / Aerobic Exercise | ≥ 70% | ≤ 50% |
Table 1 Key Quantitative Parameters for the Early Assessment of Exercise Deficit Disorder (EDD)
Early quantitative assessment of the onset of EDD provides an opportunity to tailor personalised exercise routines and diets based upon the optimisation of functional foods in accordance with individual health profiles. The values summarised in Table 1 are representative of the last five years of data collection amongst individuals participating in preventative health guidance and assistance during primary and secondary health prevention programmes. BMI = kg/m2, WHR = waist circumference / hip circumference, HRR = HR Max - HR Rest.
Establishing a quantitative parametric framework for the early assessment of EDD provides several core advantages when tailoring personalised primary and secondary preventative health programmes. These are some of the most valuable advantages:
- It provides affected individuals with an objective tool to become immediately aware of their EDD status and of its direct impact on their current health condition.
- A personalised set of blood-based tests can be performed to further determine and refine the immediate and long-term actions required to address EDD.
- Based upon the severity of EDD, a personalised Master Road Map can be structured to effectively reverse this condition and its impacts on physical and metal health status. This includes further clinical tests / studies, as required, the implementation of a personalised diet supported by functional and adjuvant foods and selective exercise routines.
- Heart and cardiovascular disorders
- Exercise Deficit Disorder (EDD)
- Overweightness and obesity
- Type 2 diabetes
- Cancer and immune disorders
- Anxiety and depression
- Fatigue
- Anxiety
- Depression
Approximately 90% of individuals suffering from EDD, particularly women, using the criteria outlined in Table 1, experience chronic constipation as determined by the measurement of Colonic Transit Time (CTT) using a combination of radiography and multiple radio opaque marker technique[8]. Individuals enrolled in primary and secondary preventative health programmes effectively reverse constipation within approximately 12 weeks. Some highlights of these personalised programmes are described in this article.
Personalised Primary and Secondary Preventative Health Programmes: Reversing EDD and Improving Physical and Mental Health During COVID-19
The occurrence of the COVID-19 pandemic outbreak and the continuous emergence of SARS-CoV-2 variants and subvariants of concern have had a sustained impact on global health with an asymmetric level of disease severity[14-16].
The asymmetric patterns of disease progression and severity have been related to a variety of health status at time of infection and to several comorbid conditions[14-17]. These include among others:
During the deployment of public health measures aimed at decreasing daily rates of SARS-CoV-2 infectivity, including stay-at-home orders and designated COVID-19 regional and differential lockdowns prior to and during early stages of mass vaccination campaigns, several public health organisations reported a sharp increase in a variety of mental health conditions and overweightness among children, adolescents and young adults[18-20].
Based upon our involvement in the investigation of the origins of and the characterization of the SARS-CoV-2 / COVID-19 pandemic outbreak since its emergence[14-16], in January of 2020, individuals that had been enrolled in personalised primary and secondary preventative health programmes were informed of the need to revisit their health status and of the risks associated with the eventual exposure to a novel respiratory virus of unknown origins.
In the months that followed, a first group of eight individuals expressed their desire to revisit their health status, in particular, due to comorbid conditions such as EDD, obesity, heart and cardiovascular disease and cancer. Some have also manifested the presence of anxiety and depression.
Interestingly, most of this first group of people had reported to follow adequate eating habits and exercise routines. Therefore, as part of the structuring of a Master Road Map to address some of their health concerns, these individuals were simply monitored during a period of 16 weeks by primarily recording their body weight and body mass index (BMI) without introducing any personalised changes. As shown in Figure 1A, during the 16-week monitoring period, none of the participants succeeded in efficiently controlling their body weight and reducing their high BMI values without the structuring of personalised diets and exercise routines.
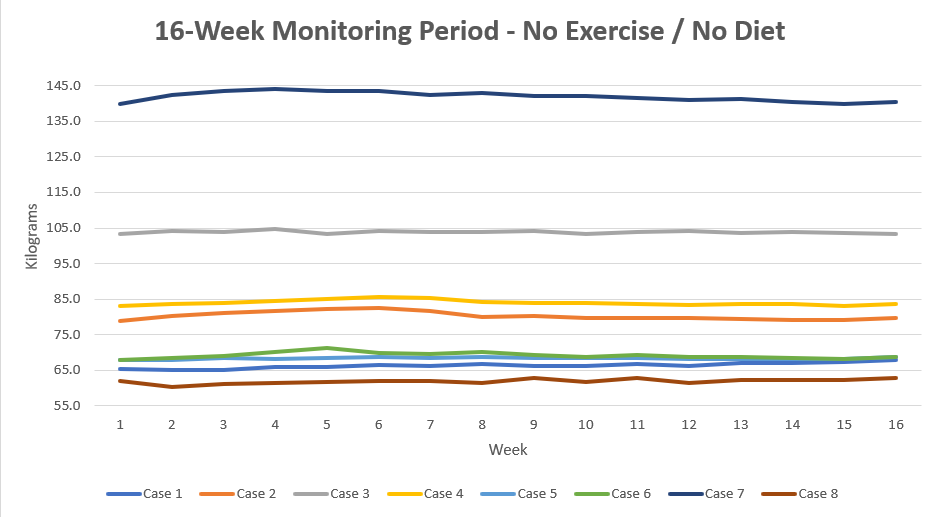
Figure 1A 16-week Monitoring Period - No Exercise / No Diet
Prior to the structuring of a personalised Master Road Map (MRM) including the clinical evaluation of individual health status, exercise routines and diet, participants interested in improving their health were monitored during a 16-week period. During that time period, no changes to their lifestyle routines in relation to their diets and weekly physical activity were implemented. No improvements in the weight and BMI values were observed.
After the completion of a 16-week monitoring period with no changes in exercise and diet, each participant was provided with an individually tailored programme that included selective functional foods, a weekly addition of a 250 ml culture of nNE active biogenic clone beverage[14] and no less than 180 minutes of combined aerobic, resistance and increased extension mobility exercise routines, each varying in intensity and duration according to individual needs. Personalised weekly adjustments of total calorie intake were also performed, ensuring that weekly weight loss did not exceed more than 2% of the initial body weight value recorded at any given time.
The direct impact of personalised exercise and diet routines on body weight loss during a 16-week monitoring period is illustrated in Figure 1B.
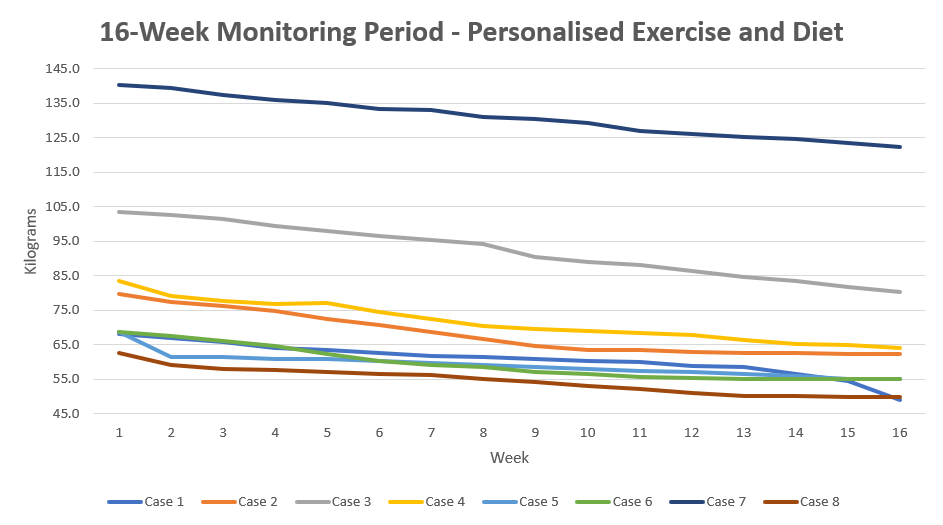
Figure 1B 16-week Monitoring Period - Personalised Exercise and Diet
After completion of a 16-week monitoring period without any changes in exercise and diet, personalised Master Road Maps (MRMs) were provided to each participant. MRMs encompassed the use of selective functional foods together with a weekly supplementation of a 250 ml culture of nNE active biogenic clone beverage[14] and no less than 180 minutes of combined aerobic, resistance and increased extension mobility exercise routines, each adjusted in intensity and duration according to individual needs.
Due to physical limitations during the stay-at-home orders and designated COVID-19 regional and differential lockdowns, part of the exercise routines was performed outdoors and coordinated through video conferencing, as required. In addition to exercise routines outlined within personalised MRMs, participants were highly encouraged to performed at least one outdoor activity of their choice every week.
The completion of 16 weeks of exercise and diet as prescribed by personalised MRMs resulted in the effective reversal of overweightness and obesity as demonstrated by the achievement of weight reduction and the achievement of healthier BMI values by comparison to those reported prior to the articulation of personalised MRMs (Figure 2).
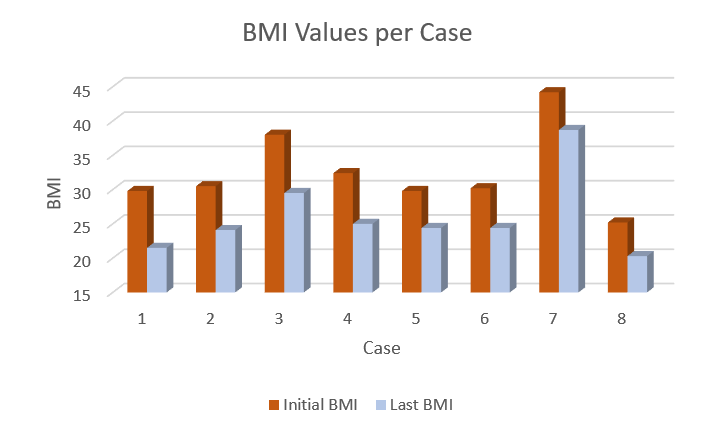
Figure 2 Impact of Personalised MRMs on Initial Body Mass Index (BMI)
In addition to the sustained weekly decrease in body weigh as shown in Figure 1B, a significant decrease in BMI values was reported in all cases after the completion of their corresponding 16-week personalised MRMs. Some participants (Cases 1, 2, 4, 5, 6 and 8) attained optimal body weighs and BMI values. During this time-period, the rest of the participants (Cases 3 and 7) were equally able to reach a healthier body weight and BMI value. These participants were encouraged to continue additional weeks until such time as optimal body weight and BMI values are achieved.
An effort was also made to monitor, weekly, overall physical and mental health status during the 16-week implementation of personalised MRMs, particularly in the context of COVID-19 public health mandates and stay-at-home orders.
Overall, participants following the 16-week personalised MRMs reported weekly improvements in their physical and mental health. These improvements included a reduction in episodes of:
Interestingly, in three out of the eight participants, although family members were diagnosed with COVID-19, none of the participants developed the disease despite having been in direct contact with more than one infected family member living in the same household. This observation is consistent with the potential protective effect of nNE active biogenic clones used as diet adjuvants due to the potential inhibitory effect on immediate viral entry accessory receptors of SARS-CoV-2[14,16]. This observation deserves closer and specific follow-up with a significantly larger sample population.
Relevance of Fostering Routine Physical Outdoor Activities During Childhood: Overcoming Adversities Due to the COVID-19 Pandemic Outbreak
Physical inactivity leading to the early onset of EDD has been found to be in close association, amongst several other factors, with the lack of regimented activities during childhood and adolescence[1-4,21-23]. Children exposed to limited and non-regimented outdoor activities at a young age are more likely to suffer from a variety of health conditions during adolescence and adult life[1-4,21-23]. It appears that this group of children is at higher risk of suffering from significant episodes of depression commencing by the age of 18 years old and younger as well as obesity, cardiovascular disorders, insulin resistance and cancer[1-4,21-23]. Participants in the 16-week exercise and diet personalised MRMs suffered from episodes of anxiety and depression, some of which had been exacerbated by a lack of clear understanding of stay-at-home orders and other preventative health measures designed to reduce exposure to SARS-CoV-2 and increased cases of COVID-19 requiring hospitalisation and intensive care. These episodes rapidly decreased during the first two weeks of implementation of personalised MRMs. During the winter, individuals were encouraged to complement their indoor-personalised exercise routines with additional outdoor activities. These activities included snowshoeing, skating and cross-country skiing. In addition, participants who reported not being able to continue their previous exercise routines within sporting facilities prior to participating in personalised MRM activities were provided with alternative indoor routines. These alternative activities did not count, however, toward the weekly number of minutes allocated according to their personalised MRMs.
The additional outdoor activities described above proved to be highly effective in fostering a greater compliance with the exercise routines structured within personalised Master Road Maps (MRMs). Outdoor skating activities were extremely efficient in increasing motivation and performance of regimented cardiovascular exercise routines while equally fostering family activities promoting outdoor physical activity in the children of participants in personalised MRMs, as well. This resulted in exploring and converting various ice and frozen bodies of water into skating surfaces (Figure 3A).

Figure 3A Additional Outdoor Activities: Skating a highly efficient supplementary activity
Constraints encountered throughout stay-at-home orders and designated COVID-19 regional and differential lockdowns led to the implementation of exercise routines performed outdoors and coordinated through video conferencing, as required. During these limitations, participants in the 16-week exercise and diet personalised MRMs were also encouraged to performed supplementary activities such as snowshoeing, skating and cross-country skiing. Skating activities were preferred by most participants, in part due to the numerous natural venues at which to perform this activity. In some neighbourhoods, non-participants, such as Lianne Walker (Lecompte), a City of Ottawa Personal Fitness Trainer, willingly cleared a snow-covered iced-water creek surface reaching a length of close to 800 metres, which was regularly used as a natural skating venue.
Six out of eight participants in the 16-week exercise and diet personalised MRMs acknowledged not having been involved in regimented exercise activities or other regular exercise during their childhood and adolescence. This is consistent with previous observations and reports related to the impact of decreased physical activity on health status during adulthood[1-4, 21-23].
Interestingly, optimal exercise routines during childhood were those that combined increased fine coordination, lower limb power and aerobic exercise. Ice- and roller-skating as well as cross-country and downhill skiing are better performed later in life when these activities are performed at a young age (Figure 3B).

Figure 3B Roller- and Ice-Skating: Strengthening fine coordination, lower limb power and aerobic exercise
Most public health measures and restrictions to prevent increased infectivity and transmission of SARS-CoV-2 are implemented during the winter. During this season, there are several outdoor activities that can be performed to prevent the early onset of Exercise Deficit Disorder (EDD). Due to the presence of several natural and man-made ice surfaces, as well as its affordability, ice-skating is an excellent outdoor activity. Skating involves fine coordination, lower limb power and aerobic exercise. This activity is better performed later in life when it is first learned at a young age.
Summation
Almost a year after our publication describing the epidemic onset of obesity and hyperobesity in north American children[1] ten years ago, the sharp and sustained lessening in physical activity in children and adult populations led to the definition and characterisation of the medical concept of exercise deficit disorder (EDD)[2,3]. Originally defined as a low level of physical activity that does not attain the minimal recommendations of daily exercise routines as prescribed by public health initiatives[2,3], the acknowledgement of EDD as a medical ailment has proven to be an important tool to establish an effective clinical road map for its prevention and treatment.
A parametric framework for the early identification, prevention and treatment of Exercise Deficit Disorder (EDD) with the goal of reducing its impact on the onset of mental and cardiovascular issues, metabolic syndrome, obesity and chronic diseases such as Type 2 diabetes and cancer was established.
The quantitative set of parameters used for the identification of EDD, as summarised in Table 1, were based upon five years of implementation of a comprehensive Global Preventive Health Platform.
In addition to the quantitative parameters described in Table 1, other relevant characteristics present in individuals identified as suffering from EDD included the presentation of episodes of anxiety and depression.
Consistent with recent reports of the impact of COVID-19 on mental health[18-20], participants in the 16-week personalised Master Road Map programmes (MRMs) also reported episodes of anxiety and depression during the 16-week monitoring period prior to the implementation of the 16-week personalised MRMs.
Nonetheless, episodes of anxiety and depression were significantly reduced after the first two weeks of implementation of the 16-week personalised MRMs. These episodes were more frequent and for an extended period as reported during the 16-week monitoring period with no personalised exercise and diet routines.
In addition to improving their mental health, participants in the 16-week personalised MRMs successfully reduced their body weight, consistently achieving between 1.5% to 2% body weight loss per week. Initial sensations of tiredness and numbness were equally resolved within the first 4-6 weeks of implementation of the 16-week personalised MRMs.
Six out of eight participants attained a normal Body Mass Index (BMI) within 16 weeks, with only two participants, Case 3 and Case 7, requiring additional weeks in order to achieve optimal body weight and normal BMI values.
Consistent with previous observations, weekly supplementation of a 250 ml culture of nNE active biogenic clone beverage[14] also conferred an additional level of protection against COVID-19.
Briefly, in three out of the eight participants, although family members contracted COVID-19, not one of the participants acquired the disease despite having been in direct contact with more than one infected family member living in the same household.
This observation is consistent with the potential protective effect of nNE active biogenic clones used as diet adjuvants due to the potential inhibitory effect on immediate viral entry accessory receptors of SARS-CoV-2[14,16]. This observation deserves closer and specific follow-up with a significantly larger sample population during a double-blind, placebo-controlled food challenge clinical trial.
In closing, the implementation of the 16-week personalised MRMs, which included selective functional foods, a weekly addition of a 250 ml culture of nNE active biogenic clone beverage[14] and no less than 180 minutes of combined aerobic, resistance and increased extension mobility exercise routines, each varying in intensity and duration according to individual needs, successfully reversed the negative impact of Exercise Deficit Disorder (EDD) on body weight and mental health during COVID-19 regional and differential lockdowns, stay-at-home orders and other related public health measures.
For reprints, please use the contact form, below, or address the corresponding author, listed above.
